State of perioperative workforce in 2023: Part 1
Takeaways
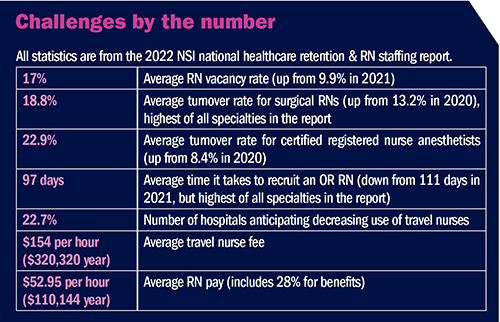
- Perioperative staffing issues are likely to continue throughout 2023 because of rising case volumes and a lack of experienced staff.
- Travelers are expected to remain a core part of staffing.
- Perioperative leaders are using multiple strategies to recruit and retain staff, including float pools for health systems that have multiple hospitals.
In 2023, perioperative nurse leaders still face unprecedented challenges, with the biggest being a lack of sufficient numbers of trained staff. OR Manager sought to know more about what leaders on the frontlines are experiencing related to the workforce, and what strategies they are using (or plan to use) in the upcoming months.
This three-part series is the outcome of conversations with leaders in hospitals and ambulatory surgery centers (ASCs) of differing sizes and locations; the information gleaned provides context for what has been published about the industry in recent months. Part 1 focuses on the hospital OR setting; a separate article on ASCs will appear in the May issue. Part 2 will examine areas outside the OR—postanesthesia care unit (PACU) and sterile processing department. The final installment will turn to OR leaders in all settings and explore how they are supporting themselves and new managers in meeting today’s challenges.
A widespread problem
Rising case volumes have contributed to staffing pressures. Nearly all the leaders OR Manager spoke with are experiencing higher case volumes that they feel will continue in upcoming months. In addition, volumes are likely to continue to rise for several years, says Rose O. Sherman, EDd, RN, MEA-BC, FAAN, a leadership expert and professor emeritus for Florida Atlantic University in Boca Raton. “There will be significant growth in the aging population over the next decade or two,” says Sherman, who has been running leadership training webinars that include perioperative leaders. Those leaders often share that patients are older and sicker than the pre-pandemic population.
As part of efforts to have sufficient staff to meet growing volumes, all the perioperative leaders interviewed for the series have budgeted for higher workforce costs so they can compete with the local market and get closer to travel nurse pay. This coincides with recent reports of large raises for nurses as a result of contract negotiations.
Organizational size does not matter when it comes to staffing issues. “Our bubble finally popped,” says Casey Orth-Nebitt, BSN, RN, CNOR, director of surgery for Buena Vista Regional Medical Center, a 34-bed rural hospital in Storm Lake, Iowa. “We’d been immune to the staffing issues that plagued others before and during the pandemic, but starting in the past 4 months, I’ve had turnover.” She has received no applications for a surgical technologist (ST) position that has been open since early November 2022.
At the same time that hospitals are facing workforce pressures and the need to increase pay, they are experiencing financial shortages due to factors such as higher supply costs and reimbursement not keeping pace with inflation. In addition, some governmental strategies that provided support to hospitals during the pandemic, such as changes in Medicare and Medicaid coverage and the Paycheck Protection Program, have slowed, ended, or will end in May.
In search of applicants
Unfortunately, an increased salary budget does not always translate into more staff, and most OR leaders report a decline in applicants for open positions. Even those willing to hire RNs and STs without previous experience are finding it difficult to fill vacant positions. “We’re down about 50% in our openings as compared to early 2022, which is good,” says Mary Anne Douglas, MS, RN, CNOR, nurse executive of surgical operations for the Canyons Region of Intermountain Health in Murray, Utah. “Although we have decreased vacancies as compared to a year ago, we are still not staffed as we were in 2019.” Douglas says the number of nurse and ST openings doubled and tripled, respectively, during the pandemic.
Hospitals of different sizes and in different locations report that finding applicants is difficult. “We have had two full-time RN positions open for over a month and have had just one applicant,” says Orth-Nebitt.
“We reached a crisis point as part of the great resignation,” says Monica Young, DNP, MBA, RN, FACHE, CNOR, CASC, NEA-BC, vice president of perioperative services for Thomas Jefferson Hospital in Philadelphia. Before the pandemic, the organization would have up to 100 candidates for the AORN Periop 101: A Core Curriculum™ Course, but that declined to between 10 and 12.
In some locations, such as where Orth-Nebitt works, contributing factors include a lack of nearby nursing and ST schools, which narrows the pipeline. In addition, “people who are graduating are looking for surgery centers where they don’t have to take call and don’t have rotating weekends,” she says and adds that one advantage of a rural setting is that those who do join the team tend to stay because of their ties to the area. Young says that many nurses do not want to take call, and they want 12-hour shifts, which organizations are unable to offer to all staff.
Perioperative leaders of hospitals in larger cities are battling a changing mindset that has made finding staff difficult. “The number of individuals wanting to come to the city instead of working in the suburbs is decreasing,” says Sarah Germanovich, MSN, RN, CNOR, TCRN, clinical practice leader for perioperative services at Thomas Jefferson Hospital. “We have to find out what will make it more meaningful for new graduates to come back to the city.”
Hospitals are using various tactics to increase the pool. Orth-Nebitt and her chief nursing officer plan to reach out to schools in other locations to see if students could complete a clinical rotation at the hospital. The hospital also offers a student nurse and a student ST internship. “We pay them a noncertified wage during their orientation until they pass their boards,” she says.
Sherman says that many ORs are hiring students and grooming them for full-time positions. “They start them with whatever little they can do and then keep building their skill set until their senior year,” she says. “That’s been successful because they get really integrated into the team.”
As a result of the decline in applicants at Thomas Jefferson Hospital, Germanovich spearheaded a proactive response that included a program to train STs (sidebar, Growing surgical technologists) and reaching out to Jefferson College of Nursing to form a partnership. The partnership consists of a 7-week perioperative rotation in the OR and other areas such as PACU and the short procedure unit. “It gives them a clear understanding as to what OR nursing is,” she says. Another option is a 3-week capstone experience for senior students, who are paired with an OR preceptor. These initiatives have helped recruit many new graduates into the OR.
Growing surgical technologists
Like many organizations, Thomas Jefferson University Hospital in Philadelphia was struggling to find and hire surgical technologists (STs). “The biggest barrier is that there are no ST schools in Philadelphia; all three that we have affiliation agreements with are in the suburbs,” says Sarah Germanovich, MSN, RN, CNOR, TCRN, clinical practice leader for perioperative services. Those in the city who might want to become an ST often cannot afford tuition and the cost of transportation to attend school and cannot afford to quit their jobs to change careers. Another problem is that although Thomas Jefferson is a clinical site for ST students, those students pass multiple hospitals on their way into town, all of which are competing for the small number of students graduating.
To widen the ST pipeline, Thomas Jefferson partnered with a training company that offers an online didactic training program for STs. The hospital, which serves as a clinical site, pays the student’s tuition and in return requires a 3-year commitment. Students spend half of their time during a week completing the didactic portion of the course, with the remainder spent in skills lab and working with a preceptor. “We have a full-time surgical tech trainer, which has been instrumental to the success of the program,” Germanovich says.
The curriculum is 18 weeks. Once students finish the didactic portion and have sufficient clinical cases, they sit for the Tech in Surgery (TS-C) certification exam offered by the National Center for Competency Testing. STs seeking this certification must complete the same number of cases required to take the Certified Surgical Technologist (CST) exam offered by the National Board of Surgical Technology and Surgical Assisting. The company the hospital works with has partnerships with schools so that students can apply credits towards an associate degree, which is required for CST certification. (Note: Some states require CST certification for STs.)
The response to the program, which was advertised on the hospital’s website, exceeded expectations, with 90 applicants in the first 5 days. “A lot of talented individuals were looking for a program like this,” Germanovich says. Word of mouth played a large role, and most of those who applied were emergency medical technicians, who have a skill set that transfers well to the OR.
The first cohort of four started as part of a pilot project in December 2022 and are expected to finish the required cases for certification in June; the second cohort started in March. “Staff have been extremely receptive, and the students have been well engaged,” Germanovich says. “I believe this program is going to be very successful.”
Monica Young, DNP, MBA, RN, FACHE, CNOR, CASC, NEA-BC, vice president of perioperative services for Thomas Jefferson Hospital, agrees. “Before we started this, our RN to tech ratio was 90 to 10, which is a costly model,” she says. “Our goal is that after the four cohorts we have planned for 2023 is to have a 70 to 30 ratio, which is a significant savings.”
Some hospitals are reaching out to those who left during the height of the pandemic to see if they would be willing to return. For example, according to a February 2023 article in Becker’s Hospital Review, Henry Ford Health has hired one in four nurses who left by offering options such as higher pay and the ability to work in different settings. The hospital used a texting campaign to contact nurses who left in the past 6 months.
Are travelers here to stay?
Reports of decreased travel nurse contracts across the country are likely due to organizations trying to reduce labor costs, but travelers remain a key staffing resource. “More and more people are resigning themselves to using travelers as part of their core staffing,” Sherman says. Some leaders in her programs have at least 50% travelers in the OR, and most of those interviewed for this series are using travelers.
“More than 50% of my workforce are agency,” says Melissa Lingle, MBA, BSN, RN, surgical services director for Mount Carmel East in Columbus, Ohio. Mount Carmel East has 13 rooms in the main OR and two rooms in the open-heart OR. Because of staffing limitations, the hospital is operating below normal levels, with current number of cases averaging about 25 to 30 per day in the main ORs and 2 to 5 in the open-heart ORs. Lingle estimates it will take several months to reduce agency levels.
Travelers can be used short term to address workforce issues. For example, Young at Thomas Jefferson Hospital says as nurses left the organization, those who stayed had to take more call and work more overtime. To address the problem, the hospital is increasing the number of full-time employees on the night shift and using its agency staff to absorb the extra case load. “We are already seeing a decrease in call hours at night, which is a significant cost savings and a huge staff satisfier,” Young says.
Perioperative leaders also are using traveler expenses to support paying internal staff more. “If we can pay nurses more and retain them, it will cut down on our use of travelers and save money in the long run,” says Douglas at Intermountain Health.
In the meantime, staff attitude toward existing travelers is key. “We have travel nurses who continuously renew their contract and have positive things to say about the hospital and staff,” Germanovich says. In addition, having staff who welcome travelers can help with recruitment. “We hope staff who left to travel will return and travelers who are looking for a position will choose us as an employer,” she says.
Getting creative with staffing
One creative staffing strategy is a float pool, such as the one used by Intermountain Health that is detailed in the article, “Maximize your staff: Developing and using successful float teams,” published in February 2023. The pool now includes STs who float between ORs, and RNs who float either between ORs or between same day surgery, PACU, and endoscopy. Staff float among hospitals within a geographic area.
Lingle says the system Mount Carmel East is part of recently added perioperative areas to its float pool. Nurses and STs in the pool can sign up to work either in any hospital in the system or only in the four Mount Carmel hospitals in Ohio. Lingle has her first pool ST working at Mount Carmel East.
Orth-Nebitt has avoided travelers because she helps out as needed and has a pool of three PRN ST staff. “Whenever I have someone leave, I ask them if they would be willing to stay as PRN because we’ve already invested in them,” she says, adding that the benefits outweigh the effort required for activities such as ensuring competencies are current. PRN staff do not have a minimum shift requirement, but if they do not work enough shifts to be helpful over a 12-month period, their status is reassessed, and they may not be kept on.
Sometimes relatively small changes can have a significant impact. Mount Carmel East is the only trauma center for the Mount Carmel system, which means on-call staff are frequently called in. In exit interviews, staff leaving for other positions frequently cited the amount of call as a major reason for their departure. In response, the hospital plans to switch from having one in-house team and two on-call teams to two in-house teams and one on-call team. “The change reduces the on-call burden significantly,” Lingle says. Because of current openings, the new model will take a year or two to fully implement, but it has been helpful for staff to know of the goal.
Kaye Reiter, MSN, RN, NE-BC, a consultant with Impact Advisers, recommends perioperative leaders ensure they have the right mix of staff to meet OR needs. “You want to make sure you have the right number of people with the right skill mix doing the right things,” she says. Reiter, who was previously vice president of perioperative services at University of Colorado Hospital in Denver, says RNs and STs should not be doing many tasks that another employee paid at a lower rate can do. “You want to keep nurses and techs working at the top of their skill level,” she says.
Planning the budget
It can be difficult to increase pay at a time when organizations are suffering from external financial pressures. “We are working on areas of cost savings to help pay for salary increases,” Douglas says. For the most part, perioperative leaders are finding C-suite support for higher workforce budgets, although it is up to the leader to educate executives on the need.
Orth-Nebitt says the administrative team uses resources such as Iowa Hospital Association data to ensure that Buena Vista Regional Medical Center stays competitive with other hospitals in the area. Wage adjustments were made for the 2021–2022 fiscal year, and she hopes to redistribute funds from the two long-time open positions to reward staff who have stayed with the hospital.
Reiter says it is important to plan for staff turnover. “I refer to it as getting ahead of the turnover curve,” she says. “By doing that, you are setting yourself up to avoid being short staffed.” Reiter acknowledges it is a fine line between hiring to accommodate for turnover and not being over staffed. She suggests leaders look at historical trends such as the turnover rate for the past few years, and determine if there are any patterns, such as seasonal variations. Leaders also should consider who might be planning to retire. “Even if you get too far ahead of the curve and over-hire in one quarter, you can lower the numbers in future quarters,” says Reiter, who also relies on AORN’s position statement on staffing and on-call practices, which details recommended minimum staffing requirements. “It gives you a mathematical breakdown that helps determine the number of FTEs you need.”
Keeping staff
Perioperative leaders report several strategies they are using or plan to use to retain staff.
Compensation. “You have to pay people what they’re worth,” Douglas says. For that reason, it is not surprising that pay adjustments are a common strategy to recruit and retain staff. For instance, because of the ST shortage, STs at Thomas Jefferson Hospital helped train all OR RNs to be able to scrub. As a result, STs now receive compensation for precepting. (RNs already received this benefit.) “Nurses and surgical techs are partners, so they deserve this,” Germanovich says. “It’s a minimal cost and helps with retention.”
Career growth. Perioperative leaders are working to ensure staff feel they are growing their skills, so they are less likely to leave the organization. “Leaders are realizing that if they are going to retain younger staff in the OR, they have to give them a variety of experiences,” Sherman says. That includes teaching nurses to scrub, circulate, and work in more than one specialty. “That’s part of trying to keep younger nurses interested in periop as a career,” she says.
Germanovich says that during the last half of 2022, Thomas Jefferson Hospital launched a “new and improved” clinical ladder. Staff sometimes perceive ladders as taking too much effort, so education about the ladder highlighted a more user-friendly approach, and that many of the points staff can earn come from activities they perform in their daily work life. Douglas at Intermountain plans to expand the OR clinical ladder to four levels, and last year enhanced the clinical ladder for STs to include higher pay levels for those working areas with higher acuity. She has already seen positive results for the ladder strategy. “In 2022, for the first time in 4 years, the turnover rate for our highest level of ST went down to 4%,” she says. “We’re paying for knowledge.”
Scheduling. Several perioperative leaders report that incorporating technology into staff scheduling is proving to be a satisfier. Staff at Thomas Jefferson Hospital use a program that allows for self-scheduling; staff also can make time-off requests, exchange shifts with peers, and respond to push notifications about upcoming open shifts.
Case scheduling also can affect staff satisfaction. Douglas says Intermountain Health is partnering with surgeons and launching a system-wide look at actual vs projected case times, so scheduling is more accurate. A pilot project at one hospital significantly reduced case delays, which resulted in less premium pay and higher staff satisfaction as a result of fewer late nights. “It made a huge difference,” Douglas says.
Orth-Nebitt says a challenge for rural hospitals is that volumes fluctuate more than at larger hospitals. “When the schedule is packed one day but you only have two cases the next, it’s hard to make the case for a full-time person,” she says. To promote staff satisfaction, Orth-Nebitt lets new staff know the schedule varies and tries to let any who stay longer one day leave early the next. Staff also receive the call rate pay when they do not work because of low census, and they still accrue paid time off.
“We had a seismic change in the healthcare workforce during the pandemic,” Douglas says. “We need to do things differently and be creative.” Pay is important but not enough, she notes. “We have to listen to what our caregivers are saying and what they want. If we do that, we’ll have the people we need to do the work that’s there.”
Unions and the workforce
“Leaders are very worried about strikes,” says Rose O. Sherman, EDd, RN, MEA-BC, FAAN, a leadership expert and professor emeritus at Florida Atlantic University in Boca Raton who runs leadership training webinars that include perioperative leaders. “Some of the inability to redesign care delivery is coming from concern about what the union reaction will be.”
Organizations’ responses to the COVID-19 pandemic escalated interest in unions. “Nurses felt abandoned by their hospitals,” says Sandy Reding, RN, president of the California Nurses Association and vice president of National Nurses United, which has nearly 225,000 members. The union saw significant growth during the pandemic.
She emphasizes that more than 90% of contracts are negotiated without a strike and that strikes are a last resort. “No one wants a strike,” says Reding, who also is a staff nurse at Bakersfield Memorial Hospital in Bakersfield, California. She says many nurses who belong to unions, including herself, have a positive relationship with their managers, and faults corporations and top-level executives for focusing too much on profits and not enough on listening to staff. “Instead of hiring high-price consultants, they should listen to their free consultants—frontline nurses who know what we need,” Reding says.
She adds that it is important for hospitals to provide incentive pay to nurses filling extra shifts, since it means time away from families, and to allow for vacations to promote work-life balance and retention. “We want adequate staffing, proper breaks, and the supplies that we need to care for our patients,” she says.
The union says the source of the nursing shortage is not a supply issue; rather, it is caused by the number of licensed nurses who are choosing not to work. According to the National Council of State Boards of Nursing, as of February 2023, about 4.6 million RNs have an active license, but May 2021 data from the US Bureau of Labor Statistics show that only 3.3 million RNs are currently employed; 1.8 million of them work in hospitals.
In a New York Times opinion article, researcher Linda Aiken, PhD, RN, FAAN, FRCN, founding director of the Center for Health Outcomes and Policy Research at the University of Pennsylvania School of Nursing, says the US has a “robust supply of nurses.” She traces the shortage to two factors: poor working conditions and “the failure of states to enact policies that establish and enforce safe nurse staffing; enable nurses to practice where they are needed, which is often across state borders; and modernize nurse licensing rules so that nurses can use their full education and expertise.”
Others say the premise that a large pool of nurses who are not currently working could be drawn back into the workforce by better wages and working conditions is not supported by data. Joanne Spetz, PhD, director for the Philip R. Lee Institute for Health Policy Studies and Brenda and Jeffrey L. Kang Presidential Chair in Health Care Finance at the University of California, San Francisco, notes that NCSBN’s 2020 workforce survey found that among the 4,198,031 RNs with active RN licenses, more than 84% were employed in nursing, only 1.9% were unemployed and seeking nursing work, and 18% were 65 years or older (many RNs maintain their license after they retire).
“In general, there are not that many nurses who are not working and might be drawn back into nursing employment with wages and improvements in working conditions,” Spetz says, who adds that other surveys have noted that among those who are not working but are not retired, most cite family responsibilities (caring for children, parents, or both) as the reason. There also are likely regional variations in pay and working conditions that affect whether nurses are willing to work in hospitals.
However, Spetz says better wages and improved working conditions are important for retention and may help draw nurses working in non-hospital jobs back into the hospital. The non-hospital setting is an important source of nurses—all of the growth in RN employment between 2019 and 2022 occurred outside of hospitals, as Douglas Staiger, PhD, Joan Sloan Dickey Third Century Professor in the Social Sciences, department of economics at Dartmouth College, noted in his February 2023 testimony to the US Senate Committee on Health, Education, Labor, and Pensions. Staiger also noted that although nursing school enrollment is up, pass rates for NCLEX have declined.
Of course, drawing nurses away from non-hospital settings leaves those employers seeking nurses, pointing to the need for a broader approach to addressing nurse workforce issues. “A combination of higher nurse graduation rates, higher pass rates on the board exams, and better working conditions are all needed to rectify the situation,” Spetz says.
Sherman says that many nurses turn to a union because they feel it is their only option for gaining a voice. “They don’t feel anyone is listening to them,” she says. “All they want is for someone to say, ‘we know we are short staffed, we know that is very tough.’” Sherman adds that a union’s view that hospital “greed” is why nurses are not being hired and paid better ignores the reality that many hospitals simply do not have the necessary funds.
Leaders also need to contend with unionization of non-nurse healthcare employees. For example, Service Employees International Union represents several types of healthcare employees in addition to nurses, including certified nursing assistants, surgical technicians, and transporters.
The takeaway is that management, union leaders, and staff need to promote honest, open communication to build trust. “You need to have open dialogue between nurses and management,” Reding says. In addition, supporting staff through fair wages and providing them with what they need to do their jobs can keep relationships positive so that patient care remains the top priority.
—Cynthia Saver, MS, RN, is president of CLS Development, Inc, Columbia, Maryland, which provides editorial services to healthcare publications.
Read Part 2 here and Part 3 here!
References
AORN. AORN position statement on perioperative staff staffing and on-call practices. 2021.
Gooch K. Nurses secure big raises; Where, how much and when. Becker’s Hosp Rev. January 2023.
NSI Nursing Solutions. NSI national health care retention & RN staffing report. 2022.





 Free Daily News
Free Daily News