Intraoperative positioning education fills knowledge void in care unit nurses
Can experience in the OR improve patient care in the postsurgical inpatient setting?
Beginning last year, the OR at Temple University Hospital, Philadelphia, started its first Periop 101 program and trained six nurses from postsurgical care units to be perioperative nurses.
During the program, the former care unit nurses found they were not familiar with a lot of the information they were receiving on patient harm associated with surgical positioning practices, including:
• extreme body positioning with devices (eg, bean bag, lateral arm board, stirrups)
• length of time a patient is kept in a position during a surgical procedure
• surgical interventions such as insufflation.
“Throughout the process, there was a lot of conversation about how they wished they had known the information they were being taught when they worked on the care unit,” Reagan Rose, BA, RN, CNOR, perioperative nurse educator, told OR Manager.
“We found out there was a real knowledge deficit between what actually happened to our patients in the OR and how we cared for them when they came back to the care unit,” adds Colleen O’Neill-Orsini, BA, RN, OR staff nurse. “We were taught to check incisions to make sure they were clean, dry, and intact, but we didn’t focus on areas of the body that could have been affected by intraoperative positioning,” she says. “A patient could have been in a lateral position for 6 hours, but we didn’t know we should be checking the hips and other pressure areas.”
Ana Velez, RN, staff nurse, noted that when she worked in the care unit, her patients would leave the floor for the OR and then a few hours later they would come back, and she had no idea what happened to them during all of those hours. “When I started learning about what happens to patients during surgery, I began feeling really bad that I hadn’t known these things before, but I thought it was only me,” says Velez. “Then we all started talking about it and found we were all feeling the same way, and decided we wanted to do something about it,” she says.
They saw an opportunity to help increase unit nurses’ awareness of what takes place in the OR and to enhance patient care on the postsurgical units by educating the nurses on how to prevent postoperative complications, such as skin breakdown or injury, nerve injury, musculoskeletal pain, and compartment syndrome, says Rose. “The whole Periop 101 group, which we call our ‘Bridge Nurses,’ was really passionate about the idea of starting a project to educate the unit nurses,” she says.
 Pre-, post-education surveys
Pre-, post-education surveys
The Bridge Nurses spearheaded the project and came up with an idea of how to measure any benefit and change in the care unit nurses’ knowledge as a result of the education.
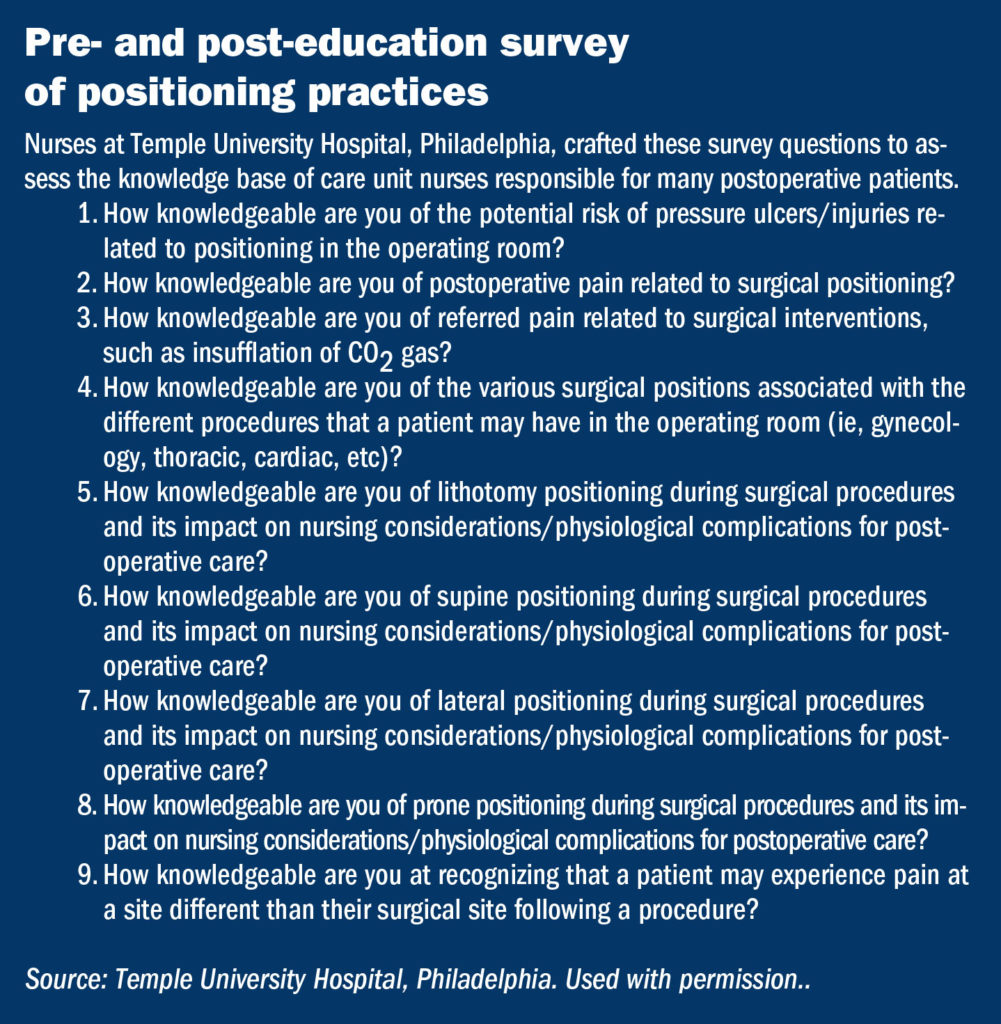
They designed nine survey questions and sent them via email to staff nurses on a small unit that received a large number of postoperative patients (sidebar at right).
“I was very proud of them,” says Rose. “I thought the survey questions were really good and reflected the care unit nurses’ knowledge of the different aspects of positioning and pain as well as potential injuries related to positioning.”
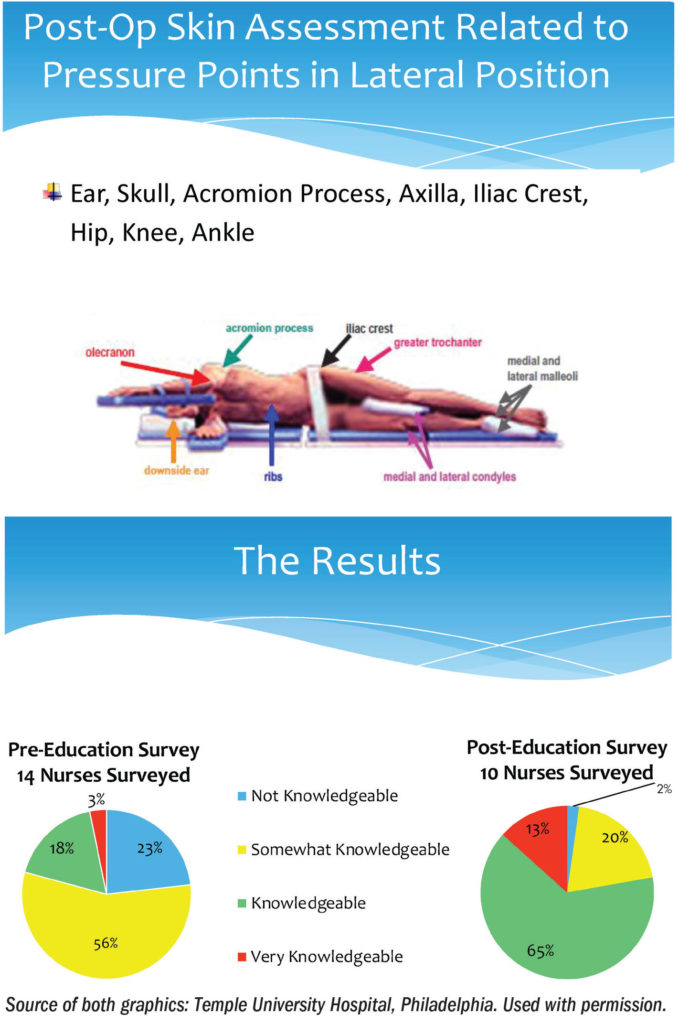
After the care unit nurses took the pre-education survey, informative posters were hung on the unit showing different positions of the surgical patient as well as pressure points in those positions (sidebar below).
The posters were made using the AORN positioning guidelines as a resource, and they hung on the unit for 6 weeks.
A PowerPoint presentation on the positions, pressure points, and potential injuries in each position also was sent via email to the nursing staff.
To determine the change in knowledge on intraoperative positioning and perioperative practices, a follow-up post-education survey was sent to the care unit nurses that contained the same questions used in the pre-education survey.
Results
The post-education survey showed an overall increase in the knowledge of risk of pressure ulcer injuries, pain related to surgical positioning, various types of surgical positioning, and referred pain from insufflation of CO2 gas.
The most significant increase in knowledge was the recognition that a patient may experience pain at a site different than the surgical site following a procedure.
After the care unit nurses received education, the percentage of those who responded that they were “not knowledgeable” decreased from 23% to 2%, indicating that 98% now had knowledge of surgical positioning, insufflation, pain, etc (sidebar above).
The change with the most significance was the increase in nurses who responded that they are “knowledgeable,” which increased from 18% to 65%.
When asked for feedback, one nurse said that learning about perioperative practices helped her understand her patients’ level of pain and what the surgical experience was like. Another said it gave him a different perspective, and he was better able to assess his patients and their needs.
Expanding to other care units

The “Bridge Nurses.” Standing, left to right: OR staff nurses Susan Rubin, RN; Hyonchu Kim, RN; Nicole Washington, RN; Courtney Sparango, RN; Ana Velez, RN; and Colleen O’Neill-Orsini, BA, RN. Lying on table: Reagan Rose, BA, RN, CNOR, perioperative nurse educator. Source: Temple University Hospital, Philadelphia. Used with permission.
Because of the encouraging results, the project has been expanded to include more postsurgical units in the hospital along with unit-specific posters. For example, the floors that receive primarily gynecological surgery patients will receive education focused on the lithotomy position and associated complications. They also are discussing making the surveys more specific for each unit.
In addition, the results of the survey were presented at a hospital-wide Nursing Grand Rounds as well as to the hospital’s Dermal Defense Team, which includes four nurses. The Dermal Defense Team does skin assessments on patients monthly and documents any skin breakdowns.
At the Nursing Grand Rounds, the attendees’ knowledge of the information that was presented was measured before and after the presentation with automated pre- and post-presentation surveys, says Nicole Washington, RN, OR staff nurse.
Susan Rubin, RN, OR staff nurse, notes that the presentation to the Dermal Defense Team was met with a lot of enthusiasm. “Even though their primary focus is skin integrity, they told us we provided them with information they didn’t know, and really welcomed the information we provided them,” Rubin says.
In the future, Rose says they hope to measure not only nurses’ knowledge but also improvement in patient outcomes once this program has been implemented on all the postsurgical care units.
Hyonchu Kim, RN, OR staff nurse, and Courtney Sparango, RN, OR staff nurse, the other members of the bridge, noted how proud they are to have been a part of this team and what they have accomplished for the patients and the nurses on the care units.
All six nurses in the bridge group continue to work in the OR and have been there for a year. ✥
References
AORN. Guideline for positioning the patient. Guidelines for Perioperative Practice 2018. 673-743.
Kim H, Orsini C O, Washington N, et al. Improving post-op care by educating floor nurses on intra-op positioning. Poster. AORN Global Surgical Conference & Expo. 2018.

 Free Daily News
Free Daily News