Munro Scale assessment helps reduce HAPI rates
Einstein Healthcare Network, Philadelphia, surgical cluster team members (left to right): Trish Brown, BSN, RN, clinical nurse PACU, surgical cluster chair; Robert Levin, MSN, RN, CNOR, RRT, clinical educator surgical services; Maureen McClellan, RN, clinical nurse preoperative and postoperative areas, surgical cluster secretary. Used with permission.
Each year, more than 2.5 million adults in the US develop pressure ulcers, according to the Agency for Healthcare Research and Quality (AHRQ). These lesions bring pain, risk for serious infection, and increased healthcare utilization.
Data on the costs of treatment vary, but some estimates range between $37,800 and $70,000 per ulcer, with total annual costs as high as $11 billion. The Centers for Medicare & Medicaid Services now considers Stage III and IV pressure ulcers a healthcare-associated condition and will not pay more for the treatment of patients who acquire them in the hospital.
These are compelling reasons for perioperative nurses to be proactive in doing risk assessments and using preventive measures to protect their patients from pressure ulcers.
At Einstein Healthcare Network’s Philadelphia campus, staff noticed an increase in hospital-acquired pressure injuries (HAPIs) in several inpatient units and began implementing changes to lower the incidence. They reported on their initiative at a network council meeting, a hospital-wide governance meeting.
“As the chair for the surgical cluster, I attended the network council meeting,” says Trish Brown, BSN, RN, clinical nurse PACU. “It was at this meeting that I learned of the increase in hospital-acquired pressure ulcers and injuries,” she says, “and I took it back to the surgical cluster to see what we could do to help improve the numbers.”
Perioperative nurses in Einstein’s surgical cluster recognized the opportunity to help their surgical patients and joined the effort, which ultimately cut the incidence almost in half.
Each service line at Einstein Healthcare Network has a cluster that consists of direct care nurses. Clusters report up to the network council, whose membership includes nursing leadership. The surgical cluster is composed of pre-, intra-, and postoperative direct care nurses, as well as a nurse manager and nurse educator.
Munro Scale
Surgical cluster members did a literature search on pressure injuries, which showed surgical patients are at especially high risk because of immobility during long procedures and anesthesia that blocks sensitivity to pain and pressure.
The search also found the Munro Pressure Ulcer Risk Assessment Scale for Perioperative Patients (Munro Scale), which is used to identify adult general surgery patients at risk for pressure ulcer development.
Cassendra Munro, MSN, RN, CNOR, Magnet & Professional Practice Manager at Providence St John’s Health Center, Santa Monica, California, created the Munro Scale specifically for surgical patients. Munro partnered with AORN to develop the scale.
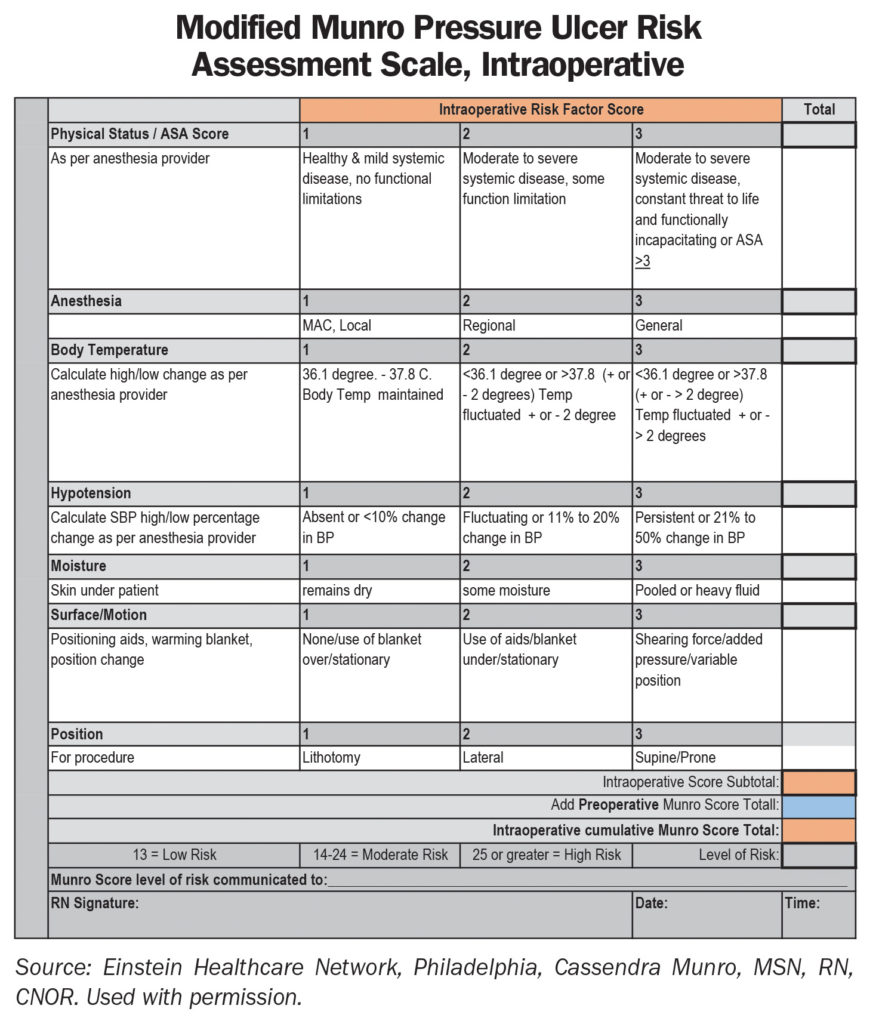
The Munro Scale assesses the patient’s risk level for each phase of surgery: preoperative, intraoperative, and postoperative. Each phase of the assessment results in a risk score of low, medium, or high, with a cumulative score at the end that is documented and communicated to the inpatient unit nurse for continuation of care.
For the project, the surgical cluster team modified the Munro Scale by assigning different colors to each phase of care to help staff carry over the risk numbers, for example, preoperative is blue, intraoperative is peach, and postoperative is green (sidebar below).
Approval for the project and modification of the scale was obtained from Munro and the chief nurse executive. Cluster members served as experts, and champions were recruited from staff. Several education sessions were provided for staff, and follow-up meetings were held with staff to address barriers and report results.
Project methods
Assessment data on the incidence of HAPIs were collected for 3 months before implementation of the Munro Scale and for 9 months after implementation.
Data also were collected on the use of the risk assessment form by staff.
“We found that our computer system could tell us preoperatively which surgical cases were expected to be 2 hours or longer,” says Maureen McClellan, RN, clinical nurse preoperative and postoperative areas, and secretary for the surgical cluster.
These patients were assessed preoperatively with the Munro Scale. Any patient whose risk assessment scale was seven or higher received a multilayered pressure dressing, and this information and assessment were then passed on to the OR nurse, notes McClellan.
After some debate, the staff decided to place the dressing in the OR when they were positioning the patients. The goal is to protect the patient, says Robert Levin, MSN, RN, CNOR, RRT, clinical educator surgical services. “If the preoperative nurses aren’t aware of a positioning factor, it is the OR nurse’s responsibility to make sure the dressing is placed on any patient with a lengthy surgery or anyone at the high-risk level.” The dressings are made for various pressure spots—the head, heels, sacrum, hips, etc.
“This project, which we did over a year, has been successful in increasing awareness of pressure injuries and decreasing their incidence in surgical patients,” says Levin.
Data for 3 months before implementation showed a 3.05% incidence of HAPIs in surgical patients, and data 6 months after implementation showed a 1.8% incidence.
McClellan says the network council and the surgical director have been very supportive. Brown says the chairman of surgery was also supportive in getting the residents to allow the nurses time to do the assessment and apply the dressings. “The chairman is happy with the results,” she says.
“We are still collecting data, and there are still some months when the incidence goes up a little, but then it goes back down,” says Brown.
“There are still some areas we can improve on, such as being more consistent in completing and using the assessment form, but we are glad for even short gains because it shows staff are thinking about pressure injuries,” says Brown.
“Another plus,” says Levin, “is that we are now going through the approval process to incorporate the Munro Scale assessment form into our electronic health record. For our pilot project, it was all on paper.”
Using the Munro Scale and preventive measures has helped cut HAPIs in surgical patients, Levin says. ✥
References
Agency for Healthcare Research and Quality. Preventing pressure ulcers in hospitals. A toolkit for improving quality of care. https://www.ahrq.gov/professionals/systems/hospital/pressureulcertoolkit/index.html.
AORN. Guideline for positioning the patient. 2018 Guidelines for Perioperative Practice. Pp 673-744.
AORN. Prevention of perioperative pressure ulcers tool kit. https://www.aorn.org/guidelines/clinical-resources/tool-kits/prevention-of-perioperative-pressure-injury-tool-kit.
Centers for Medicare & Medicaid Services. Hospital-acquired conditions. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalAcqCond/Hospital-Acquired_Conditions.html.
Chen H, et al. The incidence of pressure ulcers in surgical patients of the last 5 years: A systematic review. Wounds. 2012;24(9):234-241.
Cherry C, Moss J. Best practices for preventing hospital-acquired pressure injuries in surgical patients. AORNJ. 2011;29(1):6-26.
Engels D, et al. Pressure ulcers: Factors contributing to their development in the OR. AORNJ. 2016;103(3):271-281.
Joint Commission Resources. Under pressure: Preventing perioperative pressure injuries. The SourceTM. 2017;15(11):1, 12-15, 20-21.

 Free Daily News
Free Daily News