
Editor's Note The Centers for Medicare & Medicaid Services (CMS) is moving to eliminate its Inpatient Only (IPO) List over the next 3 years, a decision that could permanently shift more surgical procedures from hospitals to outpatient settings. According to an August 24 article from Fierce Healthcare, the policy promises…

Editor's Note: This page is a companion page to the main article, "Survey: Staffing problems increase as surgical volume continues to rise." Most OR leaders (81%) report having a business manager. Historically, fewer than half had this position (42% in 2024, 37% in 2023, and 43% in 2022). The…

Editor's Note The proposal from the Centers for Medicare & Medicaid Services (CMS) to eliminate the Medicare Inpatient Only (IPO) list over 3 years could significantly expand opportunities for ambulatory surgery centers (ASCs), with rural facilities among those positioned to benefit most, Ambulatory Surgery Center News August 12 reports. The…

Editor's Note Patients treated by hospital-affiliated physicians are far less likely to receive specialty procedures in lower-cost settings, while private-equity–affiliated doctors are the most likely to steer patients toward these options, Ambulatory Surgery Center News August 12 reports. The findings come from a Mount Sinai study that examined physician affiliation,…
For decades, ambulatory surgery centers (ASCs) have shown their ability to deliver high-quality surgical care at substantially lower cost than hospital outpatient departments (HOPDs). ASCs achieve these savings through leaner operations, streamlined staffing models, and specialty-focused efficiencies, not by compromising safety or outcomes. Studies consistently highlight procedures performed in ASCs…

Editor's Note Poor planning and rushed decisions derail too many ambulatory surgery centers (ASCs) before they open their doors. In a recent blog post, ASC consultant Emily Spooner outlined the top five errors commonly made during ASC development, offering targeted guidance on how to avoid them. According to the post,…
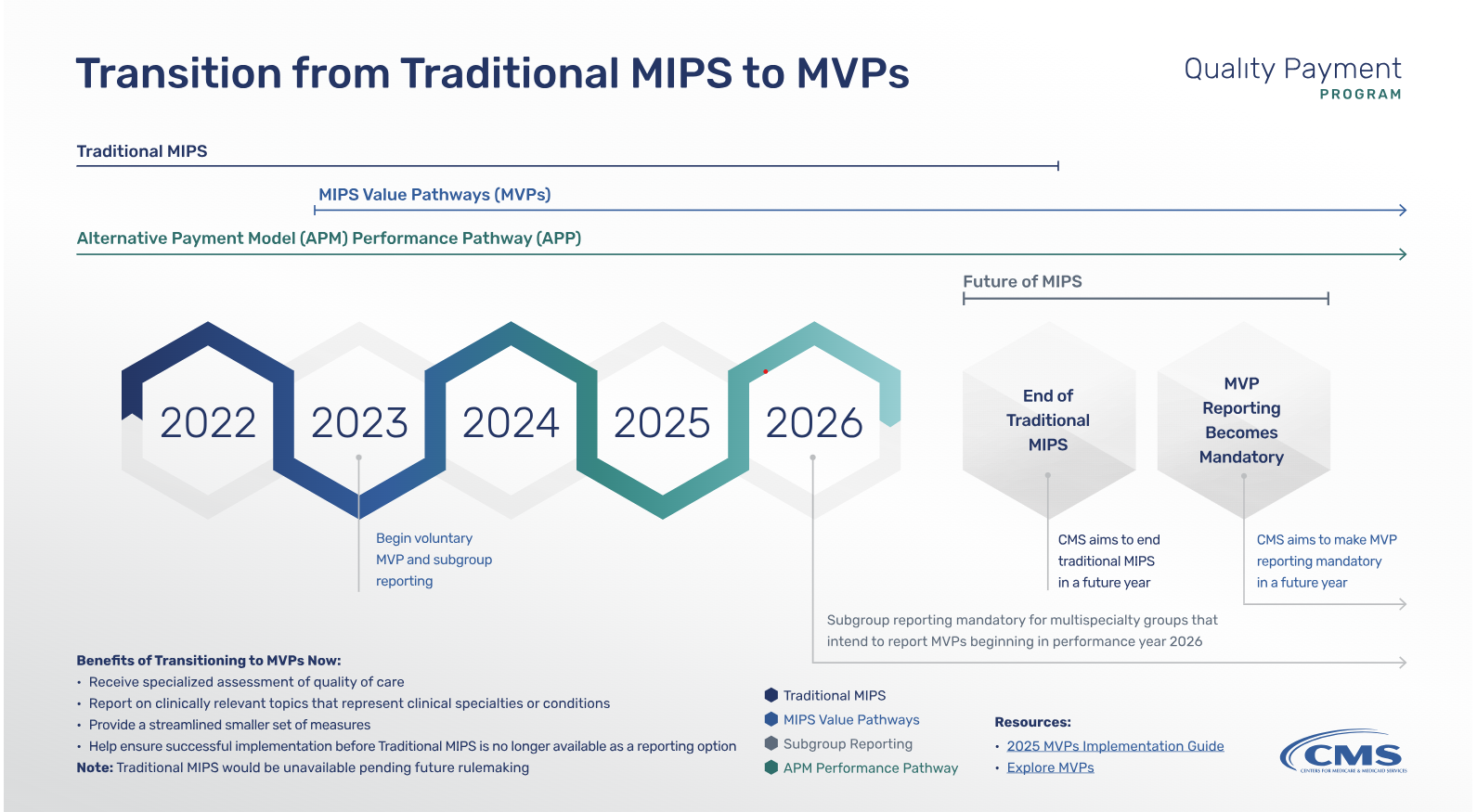
In July 2025, the Centers for Medicare & Medicaid Services (CMS) proposed sweeping changes to the Medicare Physician Fee Schedule for calendar year 2026. Among the most impactful updates is the launch of the Ambulatory Specialty Model (ASM)—a mandatory value-based payment program focused on heart failure and low back pain.…

Editor's Note As part of the Centers for Medicare and Medicaid Services (CMS) newly issued 2026 Final Rule, the Transforming Episode Accountability Model (TEAM) will hold hospitals and health systems accountable for the entire episode of care for major surgeries, from admission through 30 days post-discharge. HIT Consultant reported the…

Editor's Note Hospital-employed physicians are least likely and private equity (PE)-affiliated physicians most likely to provide care in lower-cost ambulatory surgery centers (ASCs) or offices, according to a study published July 24 in the Journal of Market Access & Health Policy These care site differences translate to substantial variation in…

Editor's Note CMS is boosting 2026 Medicare outpatient payments by 2.4%, but provider groups warn the increase barely scratches the surface of mounting financial strain. Alongside the payment bump, the agency is proposing a two-track physician reimbursement model that ties rates to value-based care participation. While some see these moves…