
Editor's Note Patient complaints against hospitals have skyrocketed, rising 79% in just 5 years and topping 14,500 in fiscal year 2024, HealthLeaders September 12 reports. The surge reflects not only mounting dissatisfaction with care experiences but also systemic oversight delays that leave concerns unaddressed, fueling mistrust in hospitals. The Centers…

Editor's Note The Centers for Medicare & Medicaid Services (CMS) is moving to eliminate its Inpatient Only (IPO) List over the next 3 years, a decision that could permanently shift more surgical procedures from hospitals to outpatient settings. According to an August 24 article from Fierce Healthcare, the policy promises…

Editor's Note The proposal from the Centers for Medicare & Medicaid Services (CMS) to eliminate the Medicare Inpatient Only (IPO) list over 3 years could significantly expand opportunities for ambulatory surgery centers (ASCs), with rural facilities among those positioned to benefit most, Ambulatory Surgery Center News August 12 reports. The…

Editor's Note Healthcare providers, payers, and analytics teams face sweeping ICD-10 changes this fall, with the 2026 code updates taking effect October 1, 2025, Wolters Kluwer July 14 reports. The release includes 614 new codes, 12 invalidations, 642 billability changes, 88 terminology revisions, and the creation of an entirely new…

Editor's Note The US Department of Justice (DOJ) has conducted the largest healthcare fraud takedown in US history, charging 324 individuals, including 96 licensed medical professionals, in schemes totaling more than $14.6 billion, HealthCare Business News July 8 reports. The nationwide crackdown involved 50 federal districts and 12 state attorneys…
For decades, ambulatory surgery centers (ASCs) have shown their ability to deliver high-quality surgical care at substantially lower cost than hospital outpatient departments (HOPDs). ASCs achieve these savings through leaner operations, streamlined staffing models, and specialty-focused efficiencies, not by compromising safety or outcomes. Studies consistently highlight procedures performed in ASCs…

As we celebrate National ASC Month, it is worth recognizing how central ambulatory surgery centers (ASCs) have become to modern healthcare. Today, there are more than 12,000 ASCs across the US, including over 6,500 Medicare-certified facilities operating some 18,800 surgical suites. With over 80% of all surgical procedures being performed…

Editor's Note Medicare Advantage (MA) patients undergoing elective surgery incurred lower costs than comparable patients in traditional Medicare (TM) without higher readmission rates and with no significant difference in mortality rates, according to a study published August 1 in JAMA Health Forum. The findings suggest that MA plans reduce surgical…

Editor's Note Hundreds of urban hospitals have obtained dual urban-rural Medicare classifications since a 2016 policy change, enabling them to qualify for reimbursement programs intended for rural providers. Fierce Healthcare reported the news August 4. As detailed in the article, a study published in Health Affairs by Johns Hopkins and…
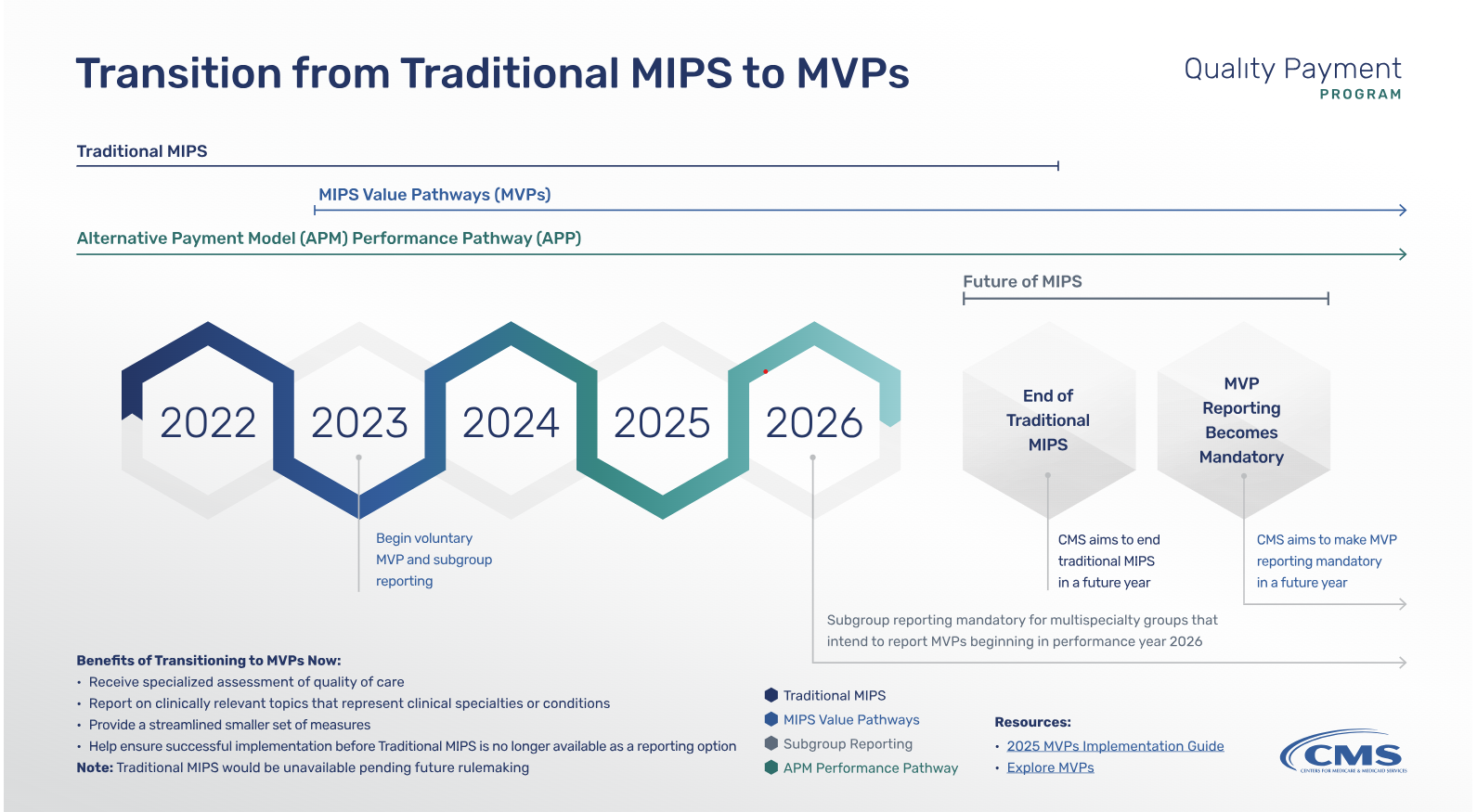
In July 2025, the Centers for Medicare & Medicaid Services (CMS) proposed sweeping changes to the Medicare Physician Fee Schedule for calendar year 2026. Among the most impactful updates is the launch of the Ambulatory Specialty Model (ASM)—a mandatory value-based payment program focused on heart failure and low back pain.…