The Munro Scale: Journey from conception to validity and reliability
After a journey of more than 20 years, validity and reliability studies for the Munro Pressure Injury Risk Assessment Scale for Perioperative Patients (Munro Scale) show that the Munro Scale works.
The Munro Scale, created by Cassendra A. Munro, PhD, MSN, RN, RNFA, CNOR, is the first standard tool that identifies perioperative patients at risk for pressure injury development.
Munro, who is a principle perioperative nurse consultant and nurse scientist at Munro Consulting, Santa Monica, California, is also the AORN liaison and chair of the Collaborating Organization Council for the National Pressure Injury Advisory Panel and is on the AORN research committee. She recently joined Stanford Health Care, Office of Research, Patient Care Services, as a nurse scientist.
Munro’s journey into pressure injury prevention began when she was starting her master’s in nursing program in 2005. She wrote a paper about patient positioning and then presented it to the class. While going through the literature review during her presentation, she noted that almost half of surgical patients can come out with a pressure injury. Her professor stopped her and asked her to repeat the surgical patient statistics, and then she asked Munro: “So what are you going to do about it?”
This question changed Munro’s life. “I set out to develop, in a scientific fashion with good scholarly rigor, an instrument that perioperative nurses could use to help improve the quality of care and patient outcomes,” says Munro. “This has been my gift to you, my passion and pursuit.”
Research methods
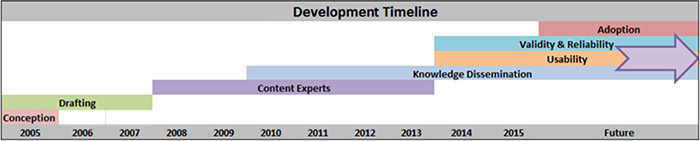
The journey of developing a risk assessment scale opened Munro’s eyes as to the length of time tool development takes, she says (sidebar, Development timeline). The timeline began with idea conception in 2005 and continues into the future.
Once Munro conceived of the idea, she used the Delphi survey method, which is a process used to arrive at a group decision by surveying experts in the field. “This method is used when you don’t have a lot of knowledge about something that you are doing,” she says. “You basically want to start off by gaining the experts’ opinions about it.”
The survey was sent out to experts, suggestions from their feedback were incorporated into the scale, and then the survey was sent out again asking for additional feedback. This was done three times, and consensus was reached that the Munro Scale did indeed indicate pressure injury risk in perioperative patients.
“For the last two of the three rounds of surveys, we knew we were nearing completion of soliciting information from our experts because we started to see a trend in the same suggestions,” says Munro. “Now the scale was ready for implementation.”
Munro also used the Middle Range Theory as a frame of reference for prevention as an intervention in the Neuman systems model. “Risk assessment, in and of itself, is an intervention for prevention,” she says. “The Munro Scale is prevention of pressure injury in the perioperative setting.”
The emphasis of the Munro Scale is on assessment of patient risk; it is not a skin assessment. It is also a documentation and communication tool.
The patient’s risk level is scored for each phase of surgery (pre-, intra-, andpostoperative), with a cumulative score that is communicated to the inpatient unit for continuation of care.
The preoperative score is based on factors such as comorbidities, nutritional status, body mass index, and mobility.
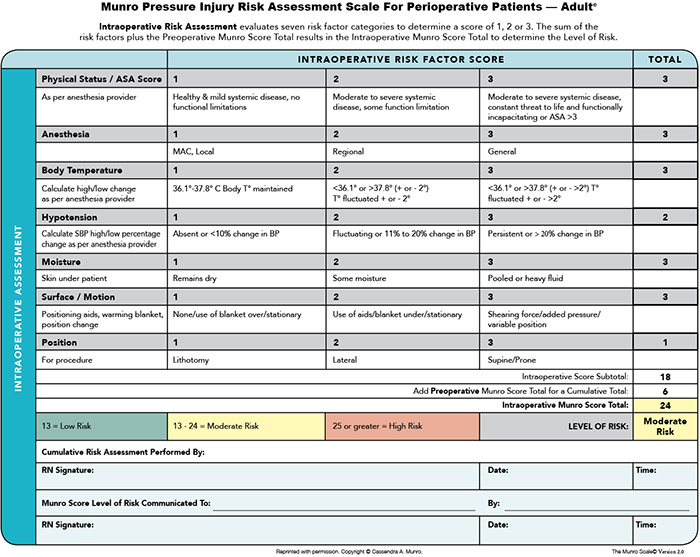
The intraoperative score encompasses components like type of anesthesia, physical status, body temperature, and hypotension (sidebar, Intraoperative risk factor score).
OR-specific risk factors include:
• use of positioning aids
• moisture on or under the patient
• friction and shear during transfers.
The postoperative score evaluates length of perioperative duration and blood loss. Because length of time spent in the perioperative unit is the most important risk factor, it is imperative to use actual time, not estimated or scheduled.
Implementation study
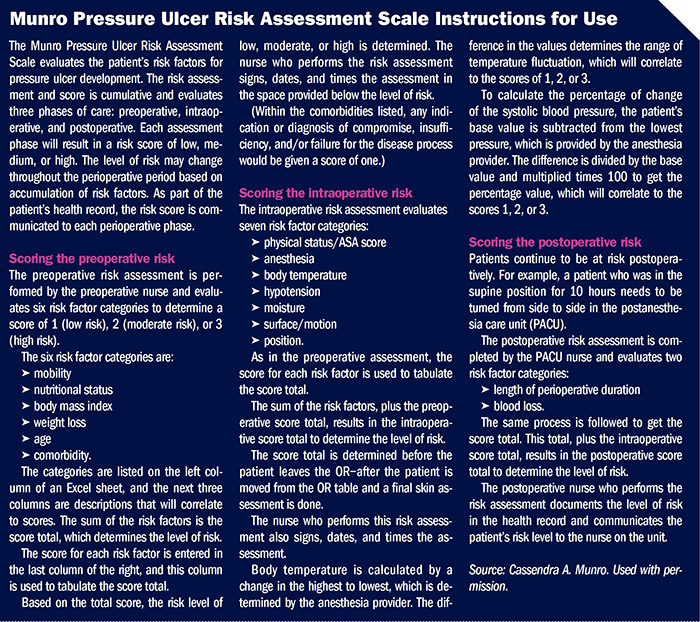
An implementation study began in 2015. Seven facilities were included. Each facility involved in the study received the following tools:
• instructions for use, which were available in a printed document and presented via a webinar (sidebar, Munro Pressure Ulcer Risk Assessment Scale Instructions for Use)
• Munro Scale
• end user feedback gathered electronically via a survey
• two case studies for practice
• references and a literature review
• two frameworks—Diffusion of Innovations Theory for the method of implementation and RE-AIM for evaluating the implementation.
Collaboration with and among the seven facilities was key, Munro says. “I could not have embarked on such a project without the assistance of the facilitators at each site. Their feedback alone was invaluable.”
Along with the implementation study, validation studies began.
CMUNRO SCALE
In 2016, the Munro Scale was made available for use in the perioperative setting to educate staff on risk factors for pressure injuries, and it was added to the AORN Prevention of Pressure Ulcers Tool Kit with the risk assessment scale.
With validation studies ongoing, Munro wanted to offer OR managers and staff use of the scale in a manner that would not only help with the education process but also could be used as a checklist to help identify patient risk factors.
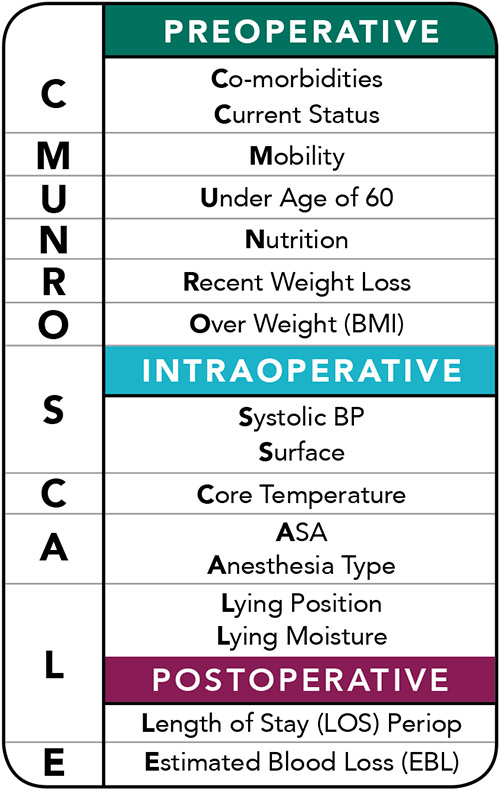
Munro came up with the idea of the mnemonic: CMUNRO SCALE (sidebar, CMUNRO SCALE). Each letter in the mnemonic is a cue for perioperative nurses to take an action, says Munro.
Preoperative assessment: The preoperative risk assessment appraises six risk factor categories that are the first word and six letters of the CMUNRO SCALE mnemonic:
• C is for comorbidity risk factors and current health status. The patient’s comorbidities are indicators of compromised skin integrity, insufficiency of defense mechanisms, failure of function of bodily organs to resist tissue breakdown, and disease processes that affect tissue perfusion and tolerance, which can lead to a pressure injury. The nurse should evaluate each of the patient’s comorbidities, consider the presence of a newly diagnosed condition, and assess the patient’s compliance with treatments.
• M represents the evaluation of the patient’s mobility status and independence.
• U poses the question of the patient’s age and whether he or she is over 60 years of age, which is higher risk.
• N is for the evaluation of the patient’s nutritional condition and nothing by mouth (NPO) status.
• R presents the question of the patient’s right weight and for the patient to recognize if he or she has had a recent weight loss.
• O represents the inquiry of the patient’s body mass index (BMI) to determine if he or she is overweight.
Intraoperative assessment: The intraoperative risk assessment appraises four risk factor categories that are the first four letters of SCALE, the second word of the acronym:
• S sets in motion the appraisal of the patient’s systolic blood pressure baseline and fluctuation throughout the surgical procedure and the surface the patient is lying on.
• C represents core body temperature that signals the effect of hypothermia and pressure injury risk.
• A refers to anesthesia type and the American Society of Anesthesiologists physical classification.
• L is paired with the lying position of the patient during the surgical procedure and the presence of moisture the patient may be lying on as a result of irrigation use, for example.
Postoperative assessment:The postoperative risk assessment evaluates two risk factor categories that are the last two letters of SCALE:
• L also represents the total length of stay (LOS) for the patient from preoperative to postoperative periods.
• E is the indicator for estimated blood loss (EBL) intraoperatively combined with sanguineous fluid postoperatively in the postanesthesia care unit.
The CMUNRO SCALE mnemonic provides a simple method for nurses to identify patient-specific and perioperative risk factors evaluated in the Munro Scale. “It was a good first step for implementing the Munro Scale because nurses would already be familiar with the actual risk factors and have a pattern for making their assessments,” she says.
Simulation modeling study
In 2018, a big step forward for the Munro Scale was a simulation modeling study to test its psychometric properties that Munro did with nurse researcher Kathleen Russell-Babin, PhD, RN, NEA-BC, ACNS-BC.
They built a model in Excel where Munro could test how a change of risk thresholds affected 1,000 simulated patient risk levels. The method allowed for exclusion of risk factors having greater uncertainties and compared two-level versus three-level outcomes.
In multivariate logistic regression analysis, Munro compared the Munro Scale (ie, count method) statistics that were generated from simulated patients to the regression method (ie, characteristics of real patients), which showed agreement in the results. “In other words,” says Munro, “they confirmed each other—the count method matched the regression method.”
The model can now create a simulated population up to 10,000 patients that is based on real patient data and characteristics, says Munro. “It is a tool that is alive and can strengthen the validity of the model itself.”
Validity and reliability evidence
During this past year Munro finished a retrospective, quantitative validity and reliability study on the Munro Scale that was the capstone for her PhD degree. The conclusions were that “the Munro Scale works—that the risk factors have some relationship to the outcome that we are tying to predict,” she says.
It is a very robust study, Munro says, and notes that she is trying to translate it quickly into something everyone can understand.
“The purpose was to explore the relationships among risk factors and whether they all help in identifying those at risk for pressure injury, and then to see what sort of prospective reliability and validity evidence we can produce from that,” she says.
Munro notes that there is some potential for removing or getting rid of some of the risk factors, but clinically speaking, she sees value in maintaining them.
She adds that there will be no removal of any of the variables until evidence shows over and over again that the Munro Scale does better without them.
An epic advancement
The most recent update for this dynamic tool is that Epic Systems Corporation (aka, Epic) is working on getting the content of the Munro Scale transitioned into a risk score with decision support in the Foundation System, which is their out-of-the-box system to allow easy adoption among community members. More information about this will be available when they get further in the development process, Munro says.
The only other electronic health record in which the Munro Scale has been implemented is AORN’s Syntegrity.
“Epic is asking for our patience, but stay on the lookout,” says Munro.
Other endorsements include:
• The Joint Commission Resources recommending implementation of the Munro Scale as a standardized process for early identification of perioperative patients at risk for pressure injuries in its 2017 issue of TheSource™.
• Upcoming publication of the simulation modeling study in the Journal of Informatics Nursing.
• AORN’s Guideline for Positioning the Patient recommending use of the Munro Scale.
• AORN adding the Munro Scale and the mnemonic, CMUNRO SCALE, to the AORN Prevention of Perioperative Pressure Injury Toolkit.
• AORN making the Munro Scale available for use via the AORN Mobile app, where it is listed as the “Munro Calculator.”
In addition, the Munro Scale has been internationally translated and implemented in hospitals in China, Italy, Turkey, and Brazil.
—Judith M. Mathias, MA, BS, RN, is clinical editor of OR Manager. Previously, she was clinical editor of AORN Journal and a cardiac surgical nurse.
References
AORN. Prevention of Perioperative Pressure Kit.
Joint Commission Resources. Under pressure: Preventing perioperative pressure injuries. The SourceTM. 2017;15(11):1, 12-15, 20-21.
Li D, Tang J, Gan X. Reliability and validity of the Munro Scale on the assessment of pressure ulcer risks in adult perioperative patients: A cross-sectional study. Int J Clin Exp. 2018;11(9):9811-9818.
Mathias J. CMUNRO SCALE created to facilitate risk assessment for pressure injuries. 2017;33(11):1, 10-11.
Mathias J. Fine-tuning the Munro Scale for pressure ulcers. OR Manager. 2015;31(6):4-5.
Mathias J. Munro Scale assessment helps reduce HAPI rates. 2018;34(12):1, 9-11.
Mathias J. Munro Scale research supports streamlining risk levels. 2018;34(9):18-19.
Mathias J. New assessment tool ready to help prevent pressure ulcers. OR Manager. 2016;32(7):1, 6-9.
Mathias J. New pressure ulcer risk tool moves forward with implementation study. OR Manager. 2014;30(7):20-21.
Mathias J. Use of refined protocols reduces pressure ulcer rates. OR Manager. 2013;29(12):1,6-8.
Munro C A. The development of a pressure ulcer risk-assessment scale for perioperative patients. AORN J. 2010;92(3):272-287.
Munro C A. The journey is the destination: Enlightenment of the Munro Scale Validation and Reliability Evidence. AORN Global Surgical Conference & Expo. 2022.
Russell-Babin K A, Law K C, Noll J C, et al. A collaborative approach for the implementation of the Munro Scale. AORN Surgical Conference & Expo. 2016.
Sengult T, Gul A, Yavuz H. Assessment of the risk of pressure ulcer during the perioperative period: Adaptation of the Munro Scale to Turkish. J Tissue Viability. 2021.


 Free Daily News
Free Daily News