Why So Delirious?
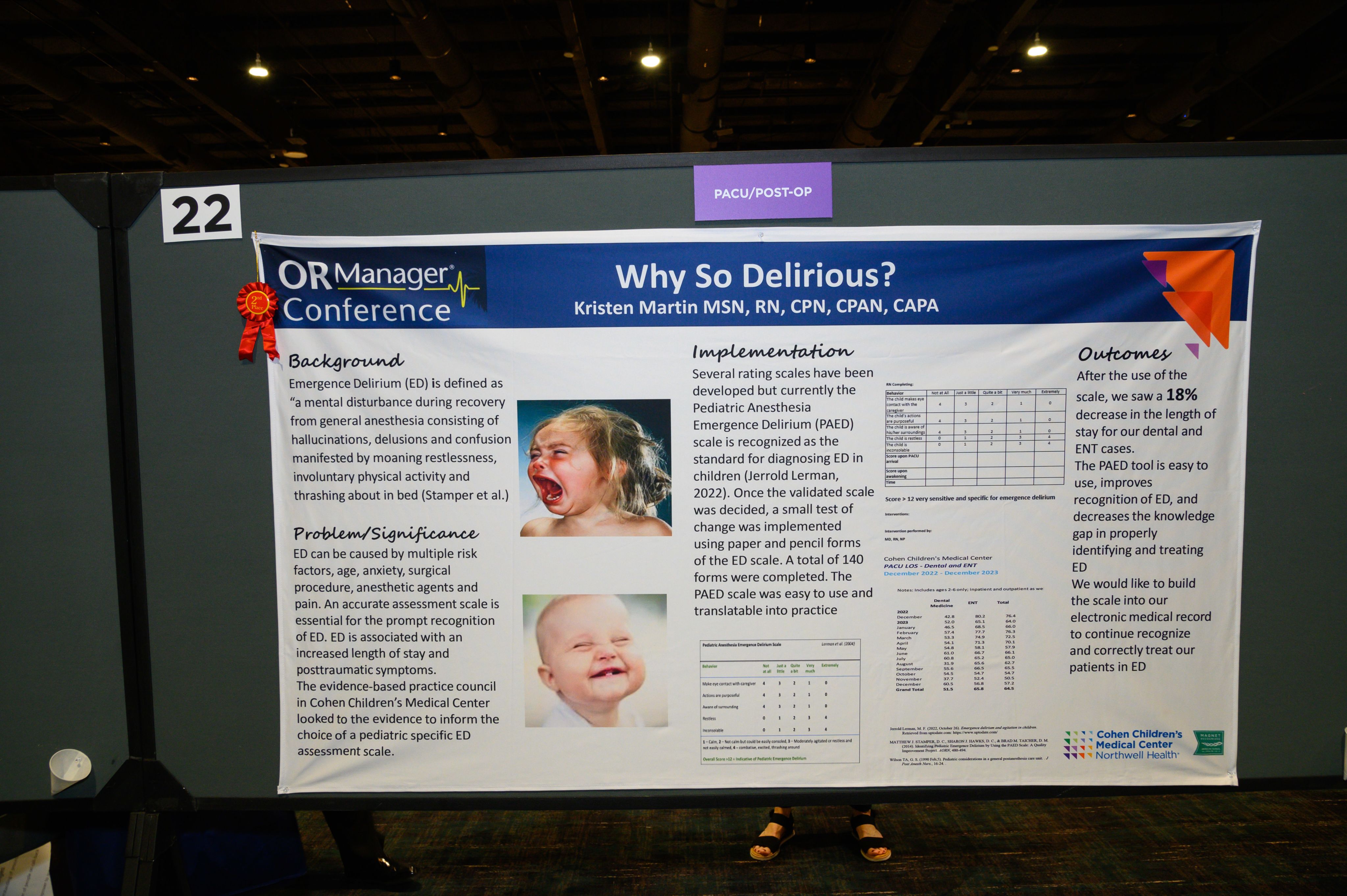
Background
Emergence Delirium (ED) is defined as “a mental disturbance during recovery from general anesthesia consisting of hallucinations, delusions and confusion manifested by moaning restlessness, involuntary physical activity and thrashing about in bed (Stamper et al.)"
Problem/Significance
ED can be caused by multiple risk factors, age, anxiety, surgical procedure, anesthetic agents and pain. An accurate assessment scale is essential for the prompt recognition of ED. ED is associated with an increased length of stay and posttraumatic symptoms. The evidence-based practice council in Cohen Children’s Medical Center looked to the evidence to inform the choice of a pediatric specific ED assessment scale.
Implementation
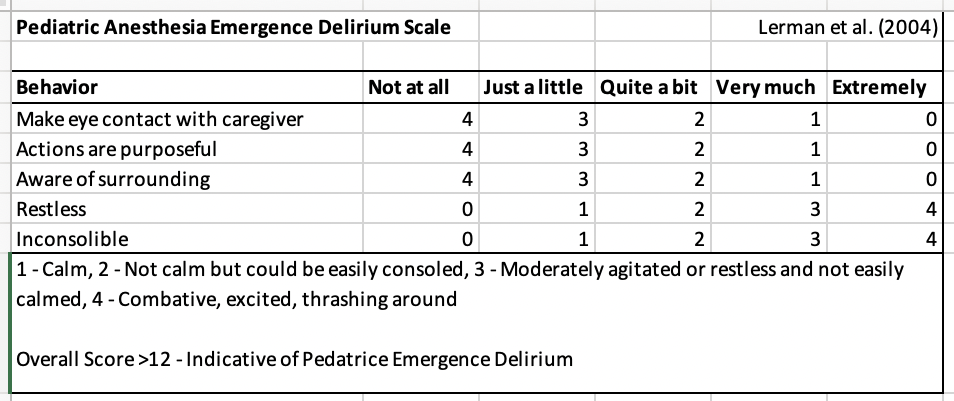
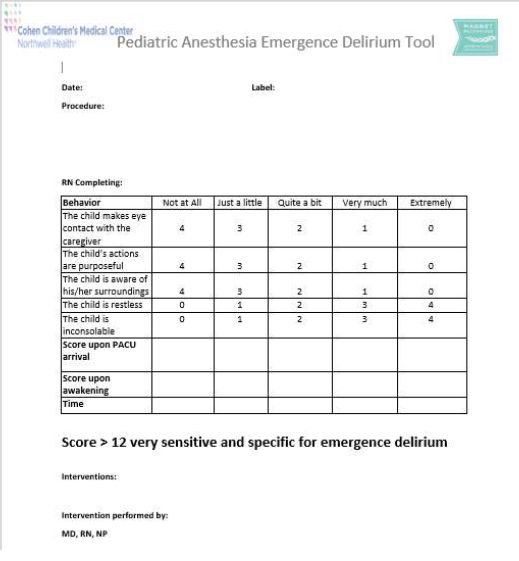
Several rating scales have been developed but currently the Pediatric Anesthesia Emergence Delirium (PAED) scale is recognized as the standard for diagnosing ED in children (Jerrold Lerman, 2022). Once the validated scale was decided, we completed a small test of change using paper and pencil forms of the ED scale. The PAED scale was easy to use and translatable into practice.
Outcomes
The PAED tool is easy to use, improves recognition of ED, and decreases the knowledge gap in properly identifying and treating ED. After the use of the scale, we saw a 18% decrease in the length of stay for our dental and ENT cases. We would like to build the scale into our electronic medical record to continue recognize and correctly treat Jerrold Lerman, M. F. (2022, October 26). Emergence delirium and agitation in children. our patients in ED.
References
Jerrold Lerman, M. F. (2022, October 26). Emergence delirium and agitation in children. our patients in ED Retrieved from uptodate.com: https://www.uptodate.com/
MATTHEW J. STAMPER, D. C., SHARON J. HAWKS, D. C., & BRAD M. TAICHER, D. M. (2014). Identifying Pediatric Emergence Delirium by Using the PAED Scale: A Quality Improvement Project. AORN, 480-494.
Wilson TA, G. S. (1990 Feb;5). Pediatric considerations in a general postanestheisa care unit. J Post Anesth Nurs., 16-24.
Presented at: