Redefining the Perioperative Experience for Children with Neurodiversity

OVERVIEW
The BEE MINDFUL™ program was developed at Cohen Children’s Medical Center to improve the care provided to children with neurodiversity such as Autism Spectrum Disorder, Attention Deficit Disorder, Sensory Processing Disorders, and Anxiety
Program Components
- Trademark Symbol for situational awareness
- Universal education for all Team Members on how to care for children with Neurodiversity
- Patient Neurobehavioral Assessment Tool (PNAT) created by content experts including parents
- BEE PASS process facilitates an expedited, calm, and safe entry into the facility
- BEE MINDFUL™ sensory Cart with sensory toys and equipment to tailor sensory needs to each patient
Expanded throughout Northwell Emergency Departments, Pediatric In-Patients, Pediatric Peri-Operative Services, Pediatric and Adult Dental, and Behavioral Health Facilities
Nationally recognized as the American Nurses Credentialing Center 2020 Magnet© prize winner


PROCESS
- Screening and inclusion into the BEE MINDFUL program in pre-surgical testing
- Interventions to promote a positive experience identified in pre-surgical testing
- Pre-op phone call with a review of interventions and to provide support to the patient and family
- Day of surgery- BEE PASS entry into the facility
- Situational awareness signage and individualized interventions incorporated into pre-op, intra-op, and post-op care
- BEE Cart use of sensory items

Measures
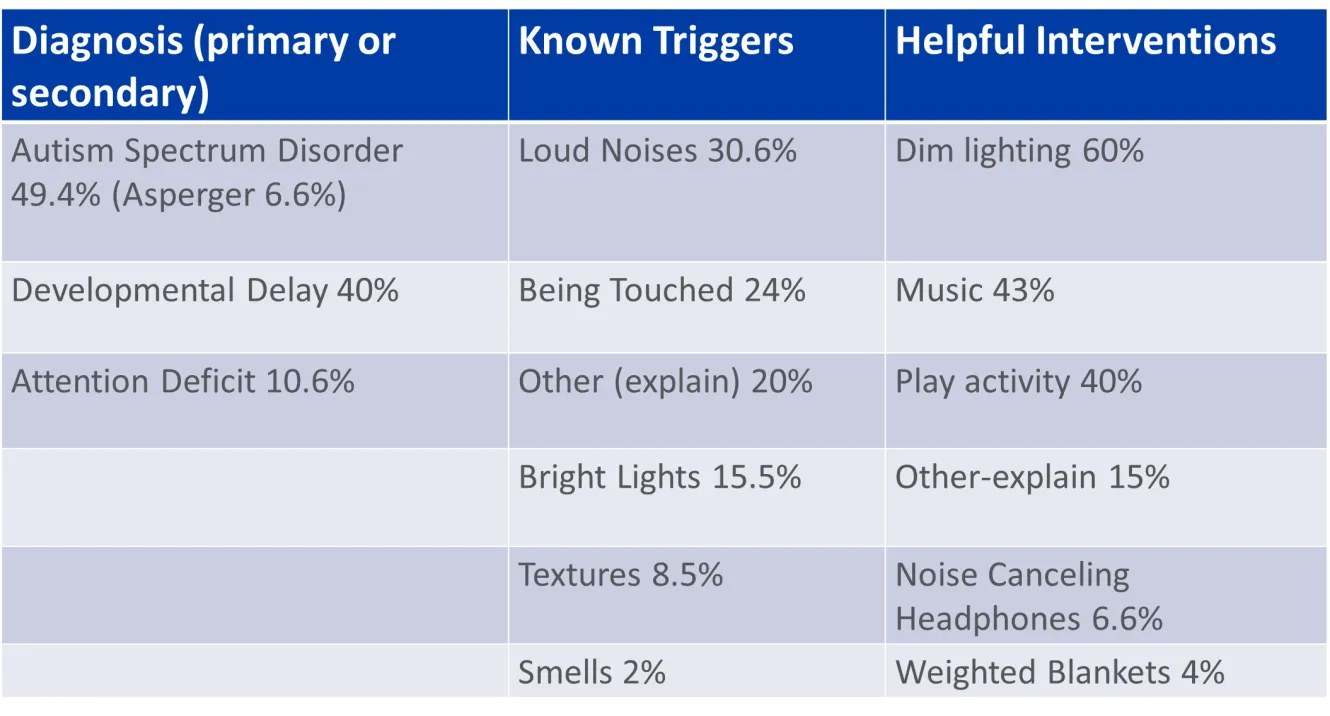
Understanding the needs of children with neurodiversity in the medical setting can help improve outcomes, decrease length of stay, provide access to care, and promote wellness.

OUTCOMES
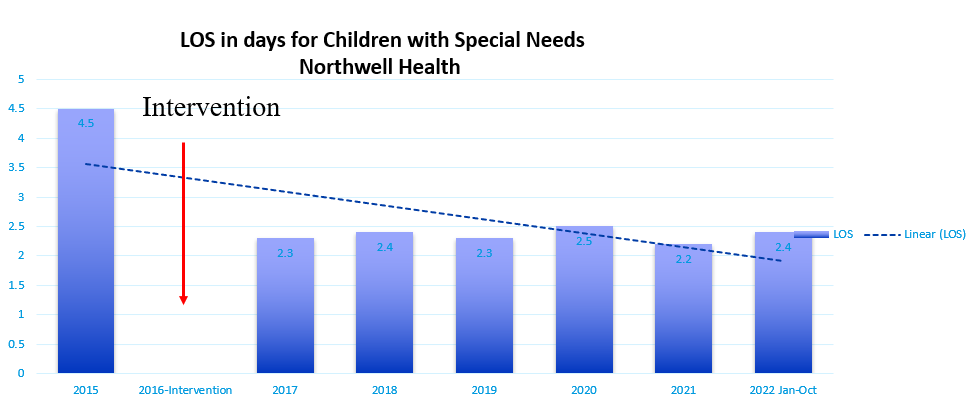
Length of stay decreased by 2.4 days and sustained over 5 years Press Ganey Survey- Initial Outcomes
"Staff addressing personal issues" 4.3% Increase
Child HCAPS- Ongoing Outcomes "Nurses listen carefully to your child" 5.4% increase
"Things that a family might know best" 5.3% increase
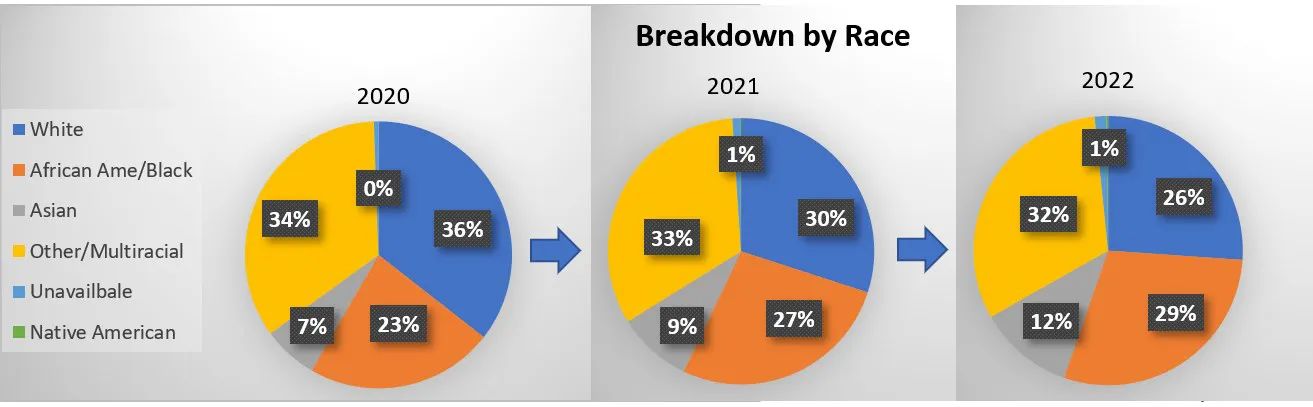
Increased diversity of children cared for with neurodiversity
- 6% increase in African American/Black
- 5% increase in Asian
NEXT STEPS
- Continued expansion of the BEE MINDFUL™ program nationally and internationally.
- Expansion of the BEE MINDFUL.com Website to include Community-based resources
References
Erwin, J., Paisi, M., Neill, S., Burns, L., Vassallo, I., Nelder , A., ... & Witton, R. (2022). Factors influencing oral health behaviours, access and delivery of dental care for autistic childre and adolescents: A mixed‐methods systematic review. Health Expectations, 25(4), 126
Harwell, C., & Bradley, E. (2019). Caring for children with autism in the emergency department. Pediatric Annals, 48(8), e333-e336.
Healthy people 2030. (n.d.). Retrieved October 1, 2022, from https://health.gov/healthypeople
Litwin, S., & Sellen, K. (2022). Designing a Sensory Kit to Improve the Environment for Children with Autism Spectrum Disorder in the Pediatric Emergency Department. Journal of Autism and Developmental Disorders, 1-11.
Straus, J., Coburn, S., Maskell, S., Pappagianopoulos, J., & Cantrell, K. (2019). Medical encounters for youth with autism spectrum disorder: a comprehensive review of environmental considerations and interventions. Clinical Medicine Insights: Pediatrics, 13, 1179556519842816.

Presented at: